A Patent Foramen Ovale (PFO) is a slit-like defect resulting from an incomplete fusion of the foramen ovale within the atrial septum. Studies show that 20-25% of the population have a PFO and echocardiography is often used to diagnosis it. This week we will review the 4 things needed to rule out a PFO during an echo bubble study.
PATENT FORAMEN OVALE (PFO)
- Incomplete fusion of the foramen ovale
- Not a true deficiency (separation) of the atrial septal tissue
- Slit-like defect
PFO: Risks & Symptoms
- Migraine headaches
- TIA, CVA
ECHO BUBBLE STUDY
We have written extensively on the correct techniques to perform an echo bubble study. Please review our past blogs here:
- 7 Indications for an Echo Bubble Study
- 9 Steps to Perform an Echo Bubble Study
- 6 Tips to Improve an Echo Bubble Study!
PATENT FORAMEN OVALE (PFO) AND ECHO BUBBLE STUDIES
- Echo bubble studies are the principal means of diagnosis
- Potential for misinterpretation (false positive and/false negative)
Positive PFO Shunt
- Appearance of micro-bubbles on the left side of the heart after their appearance in the right heart chambers
- First, inject saline without Valsalva to look for a resting shunt
Resting PFO Shunt
- Resting study: Bubble study without Valsalva
- Resting shunt: Agitated saline crosses from right-left without Valsalva
- A resting shunt has:
- Worse outcomes
- Predictor for stroke recurrence
Valsalva PFO Shunt
- If the first injection of agitated saline produces a positive result then there is no need for further imaging
- If the first injection is negative: Repeat with Valsalva
Valsalva Timing
- Injection: Performed while the patient is bearing down
- Valsalva Release: As contrast enters the RA
- Complete opacification of the RA occurs at the end of Valsalva

Valsalva Mechanism
- Valsalva momentarily alters the pressure gradient between the left and right atria
- This causes the septum primum, on the left side of the atrial septum, to transiently lift up and open the septum – like a door jam
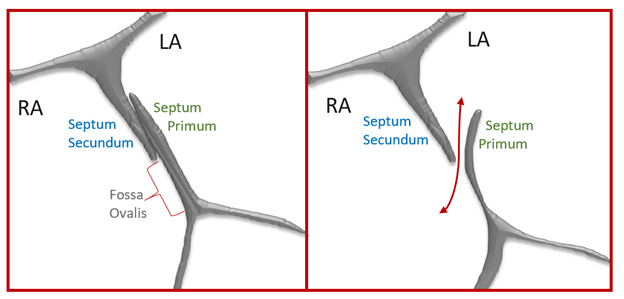
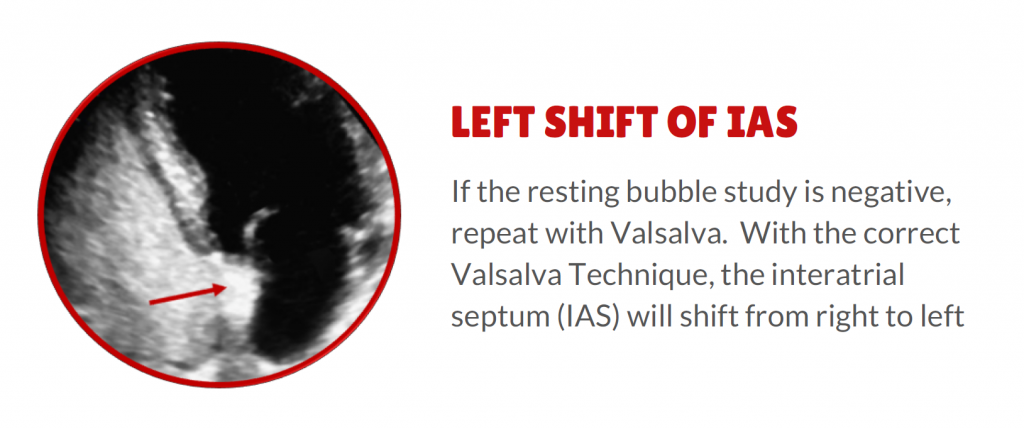
Acceptable Valsalva
- The interatrial septum shifts to the left
- An incorrect technique results in a lower detection rate of PFOs in echo
Valsalva Tips
- The patient bears down for 5–10 seconds
- Press on the patients’ abdomen and ask the patient to use their abdominal muscles to push back against your hand
- The patient may need several practice attempts
- Valsalva TEE
- Valsalva during TEE is dependent on the level of sedation
- Ask the patient to cough forcefully several times
- Perform the agitated bubble study toward the end of the TEE (patient less sedated)
Timing
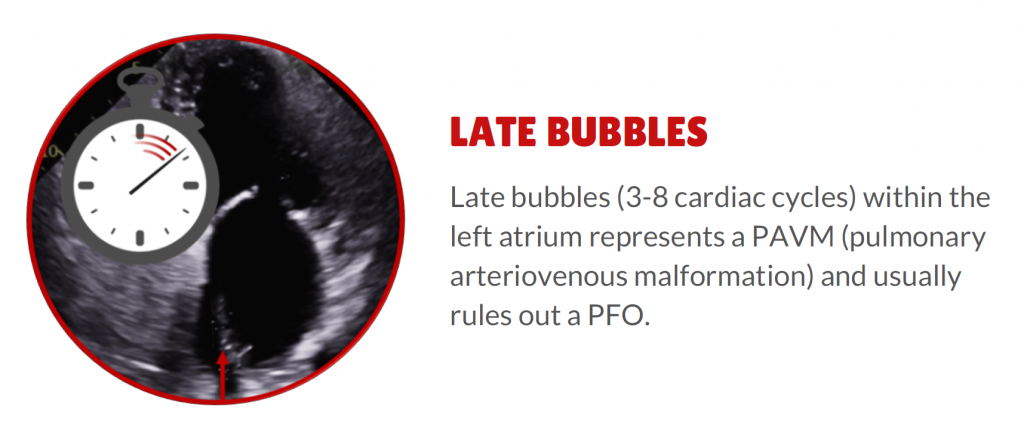
- The common viewpoint is that bubbles must appear in the left atrium within 3 cardiac cycles of their appearance in the right atrium to diagnose a PFO and that bubbles appearing in the LA beyond five cycles suggest transpulmonary shunting
Exceptions
- PFO > 3-5 seconds– dilated fibrillating atria
- Pulmonary shunt < 3-5 seconds – large pulmonary shunt may allow bubbles to get to the LA within the 3–5 cycles
FALSE NEGATIVE PFO: ECHO BUBBLE STUDY
The main reason for a false negative study is because of inadequate technique. In order to feel confident in your diagnosis to rule out a PFO with an Echo Bubble Study there are 4 things to keep in mind:
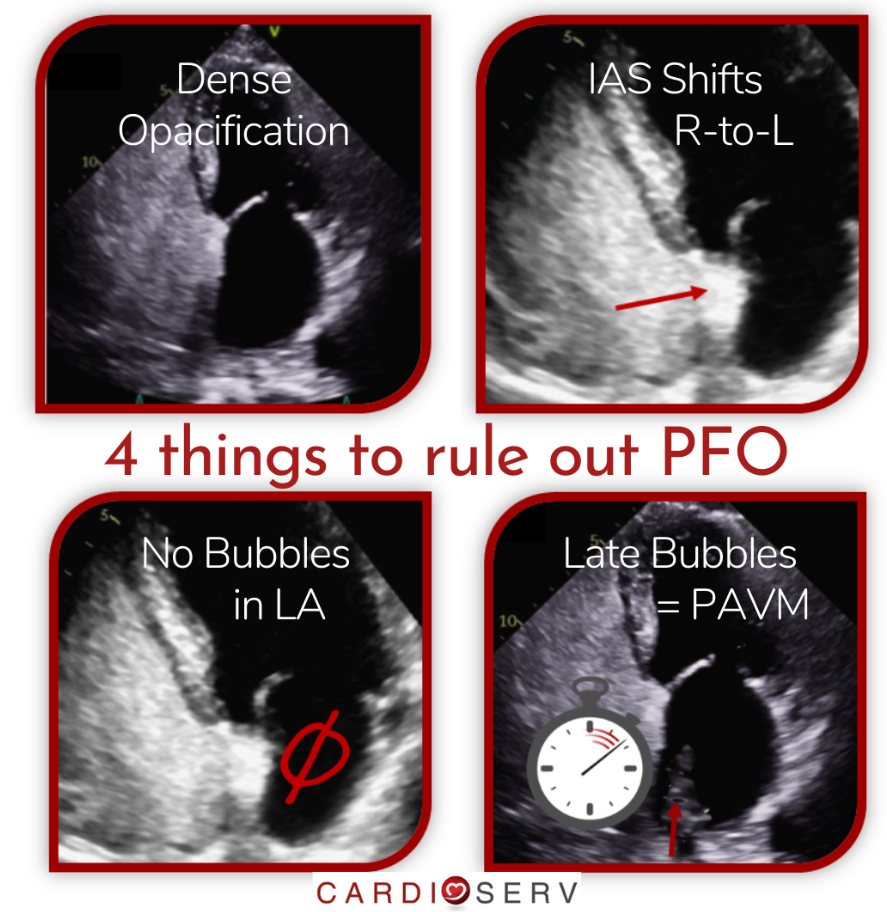
ECHO BUBBLE STUDY: 4 THINGS NEEDED TO RULE OUT A PFO
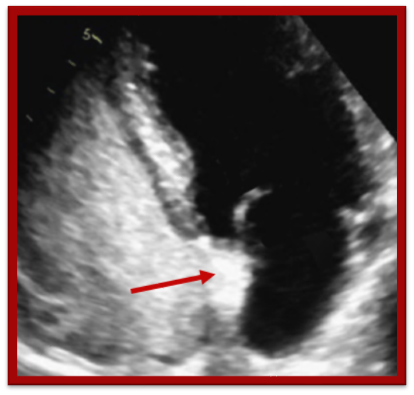
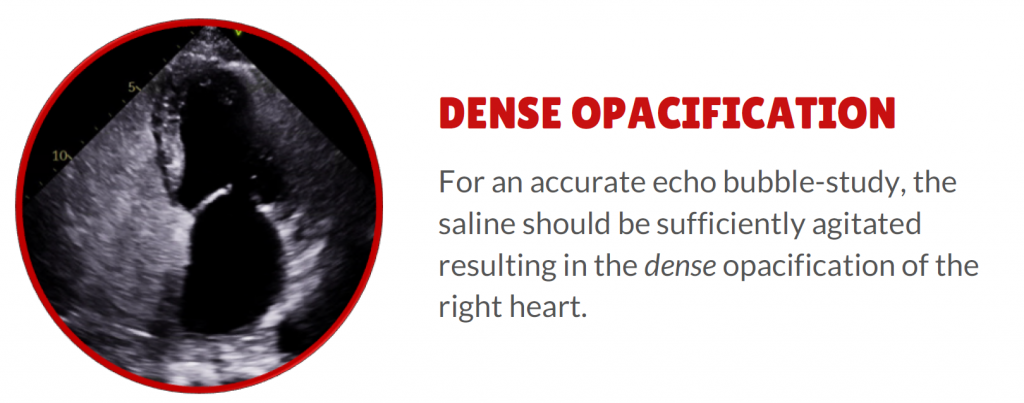
#1. Dense opacification. It is important to make sure the agitated saline was prepared correctly and administered in such a way as to densely opacify the right heart.
#2. IAS Shift. The interatrial septum should visibly shift from right to left ensuring the Valsalva was correctly performed.
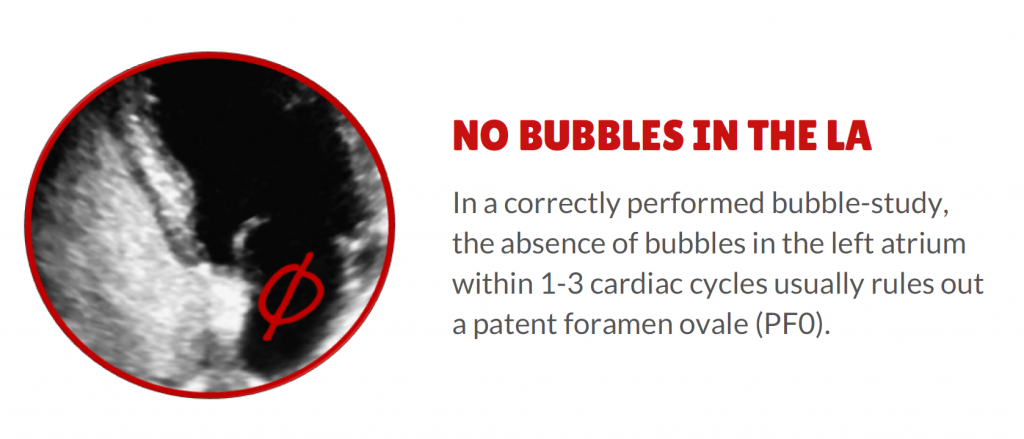
#3. No bubbles in the LA. If there is dense opacification of the right heart and an IAS shift (R-L) and no bubbles in the right atrium within 3 cardiac cycles you can rule out PFO
#4. Late Bubbles. If bubbles appear in the left atrium after 3 cardiac cycles (3-8 cycles) this represents a pulmonary arteriovenous malformation (PAVM) and usually rules out PFOs.
ECHO BUBBLE STUDY V. COLOR DOPPLER
In a study by Marriott (2013):
- 1162 patients who underwent TTE agitated saline bubble studies
- Agitated bubble and Valsalva maneuver was compared with color flow
- 403 studies had shunting but 48% were only positive with Valsalva
- Strong agreement with TEE findings
- TTE color was insensitive (22% accurate) for detection of PFO compared with agitated saline bubble study
Transthoracic color flow imaging is too insensitive for PFO screening. An agitated saline bubble study is simple and highly accurate for the detection of right-to-left atrial communication with correctly performed Valsalva
CONCLUSION
It is recommended to use an echo-bubble study with Valsalva as the primary diagnostic tool for the detection of PFO in clinical practice.
LEARN MORE ABOUT ECHO BUBBLE STUDIES AND EARN CMES
2.5 CME The Why and How of Echo Bubble Studies
- Preparation and administration of agitated saline
- Tips for improving imaging
- PFOs
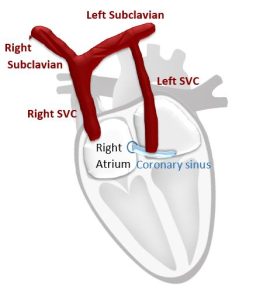
- Persistent Left Superior Vena Cava
- Pulmonary Arteriovenous Malformation
- Guided procedures bubble studies
References
- Gupta, S. K., Shetkar, S. S., & Ramakrishnan, S. (2015). Saline Contrast Echocardiography in the Era of Multimodality Imaging — Importance of “ Bubbling It Right .” Echocardiography, 1707–1719. https://doi.org/10.1111/echo.13035
- Marriott, K., Ultrasound, M. C., Manins, V., Forshaw, A., Ultrasound, M. C., Wright, J., & Pascoe, R. (2013). Detection of Right-to-Left Atrial Communication Using Agitated Saline Contrast Imaging : Experience with 1162 Patients and Recommendations for Echocardiography. Journal of the American Society of Echocardiography, 26(1), 96–102. https://doi.org/10.1016/j.echo.2012.09.007
- Porter, T. R., Abdelmoneim, S., Belcik, J. T., Mcculloch, M. L., Mulvagh, S. L., Olson, J. J., … Wei, K. (2014). Guidelines for the Cardiac Sonographer in the Performance of Contrast Echocardiography : A Focused Update from the American Society of Echocardiography. Journal of the American Society of Echocardiography, 27(8), 797–810. https://doi.org/10.1016/j.echo.2014.05.011
- Puledda, F., Toscano, M., Pieroni, A., Veneroso, G., Piero, V. Di, & Vicenzini, E. (2016). Right-to-left shunt detection sensitivity with air – saline and air – succinil gelatin transcranial Doppler. International Journal of Stroke, 11(2), 229–238. https://doi.org/10.1177/1747493015609938
- Superiority of the Combination of Blood and Agitated Saline for Routine Contrast Enhancement
Fan, Sandra et al. Journal of the American Society of Echocardiography, Volume 12, Issue 2, 94 – 98 - Romero, R., Frey, J. L., Schwamm, L. H., Demaerschalk, B. M., Chaliki, H. P., Parikh, G., … Babikian, V. L. (2009). Cerebral Ischemic Events Associated With ‘ Bubble Study ’ for Identification of Right to Left Shunts. Stroke, 2342–2348. https://doi.org/10.1161/STROKEAHA.109.549683