Last week, we shared our new year resolutions which including writing more and inspiring more. So I am jumping right in by writing a blog on the correct method to estimate right atrial pressures (RAP) when calculating your RVSP during an echo. The American Society of Echocardiography has outlined the correct use of the Collapsibility Index to estimate RAP yet the majority of the echocardiograms that we review on a daily basis still have an RAP of 10 entered for every echo. After speaking with sonographers, most admit it’s either a bad habit or it is just what they were taught to do.
Here at CardioServ we love to improve the quality of echocardiography and we feel that if we can simplify the correct way to estimate the RAP it will make it easier for sonographers to implement the correct technique into their lab and daily practice. This week we will share 8 Things to Know about estimating the RAP via echocardiography.
This blog will answer the following questions:
- Why estimate the RAP?
- What does the IVC have to do with RAP?
- What is the Collapsibility Index?
- How do you correctly measure the IVC?
- How do you accurately assess IVC collapsibility?
- Why should the patient perform a sniff?
- How do you assign the RAP value?
- What is the RAP reference range?
WHY ESTIMATE THE RAP?
During every echo we perform we routinely calculate the patient’s RVSP. We assess for tricuspid regurgitation (TR) and we measure the peak TR velocity. We usually do this without thinking and we can all robotically repeat the formula RVSP = 4V² + RAP. Unfortunately, somewhere along our journey of mastering echocardiography we may sometimes find ourselves replacing the estimation of RAP with a constant number of 10 (RVSP = 4V² + 10).
Why does it matter if we just use the value of 10 for every patient? What’s the big deal?
My answer to that would be a quick reminder that the reason we even bother to calculate the RVSP on every patient is because the RVSP is used to help determine if a patient has pulmonary hypertension. The accurateness of our RVSP calculations is dependent on how closely we estimate the patient’s true right atrial pressure (RAP). If we over-call or under-call the patients’ true right atrial pressure by using the constant value of 10 we will over/under call the severity of pulmonary hypertension.
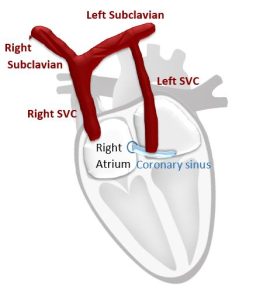
WHAT DOES THE IVC HAVE TO DO WITH RAP?
The short answer would be that the assessment of the IVC helps to determine central venous pressure and central venous pressure is synonymous with RAP. In addition to providing you with a more accurate estimate of RAP, assessment of the IVC helps assess the patients’ volume status which is important for therapeutic decision making especially in heart failure patients. All routine echocardiograms should therefore include assessment of the IVC.
WHAT IS THE COLLAPSIBILITY INDEX?
The Collapsibility Index is the relationship between the diameter of the IVC and the percent decrease (collapse) of the IVC during inspiration. This is used to determine the RAP. For simplicity the ASE suggests using specific values or RA pressure rather than ranges. To correctly use the Collapsibility Index you will need to know the best techniques to correctly measure the IVC and how to accurately assess the collapsibility of the IVC during inspiration.
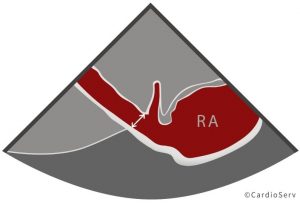
HOW TO CORRECTLY MEASURE THE IVC
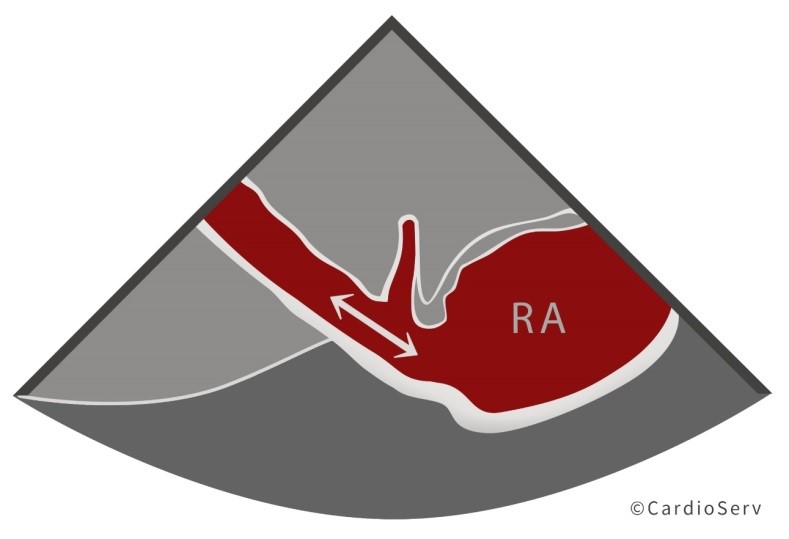
| Subcostal windowLong axis view of the IVCOpen up IVC so the diameter is at its fullest the entire length of the IVCShow IVC emptying into the right atriumMeasure the diameter 1-2 cm away from the right atrium | 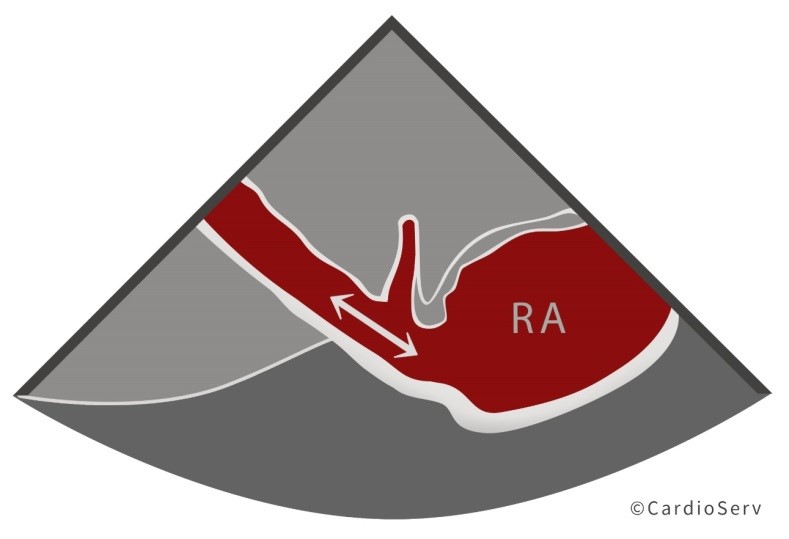 |
| Be sure to measure Inner-to-Inner Edge (I-I)Measure perpendicular to the vesselThe IVC should NOT be measured at the junction if the IVC and RA | 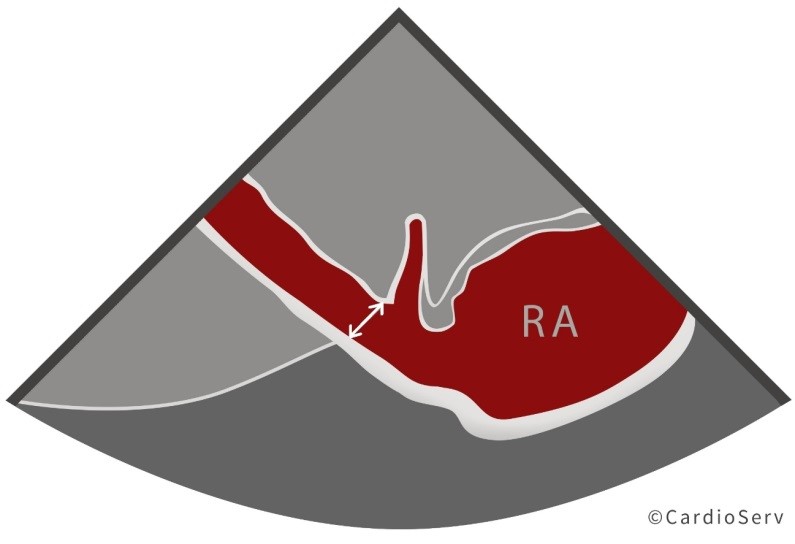 |
HOW TO ACCURATELY ASSESS IVC COLLAPSIBILITY
| M-Mode is an excellent method for displaying the degree of IVC inspiratory collapseM-Mode allows for better interrogation of the IVC over time and displays: pre sniff, sniff and post sniff views in the same imageThe IVC should NOT be measured at the junction of the IVC and RA as the degree of inspiratory collapse is less than at a more caudally located sitePlace the M-Mode cursor 1-2cm away from the right atriumObserve if the IVC collapses more than 50% | 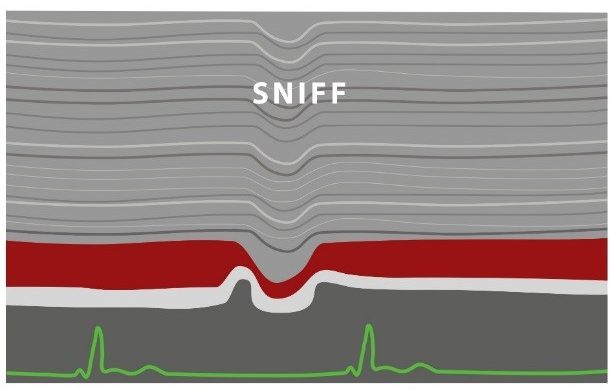 |
WHY SHOULD THE PATIENT PERFORM A SNIFF?
It is necessary to have the patient perform a sniff during the evaluation of the IVC. This is in order to determine the degree of IVC collapse. This inspiratory maneuver causes a decrease in the intrathoracic pressure while simultaneously increasing the abdominal pressure which causes the blood to flow quickly from the IVC into the right atrium. This brief and sudden emptying of blood from the IVC to the right atrium causes the IVC to briefly collapse. The sniff is preferred instead of a normal inspiration as a normal inspiration will not cause sufficient collapse of the IVC.
HOW TO ASSIGN THE RAP VALUE
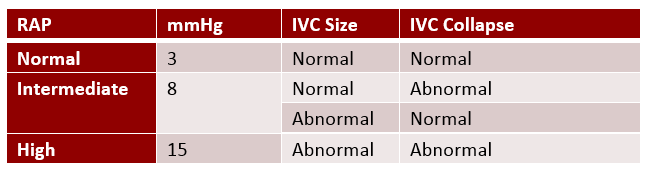
The easiest way to remember the specific RAP values is to understand the opposite ends of the RAP spectrum – the normal versus high pressure. Everything else will just fall into the middle category.
NORMAL RAP = 3 MMHG
- Normal right atrial pressure is assigned when the IVC is normal in size and collapsibility.
- IVC < 2.1cm
- IVC collapses more than 50% with sniff
HIGH RAP = 15 MMHG
- High right atrial pressure is assigned when the IVC is dilated and does not collapse normally.
- IVC > 2.1cm
- IVC collapses less than 50% with sniff
INTERMEDIATE RAP = 8 MMHG
- A middle value of 8mmHg is assigned in any scenario that doesn’t meet the normal and high values.
- For example, in a patient that has a dilated IVC but demonstrates normal collapsibility or vice versa, normal IVC size but abnormal collapsibility.
REFERENCE TABLE
Look at that! You just learned 8 correct tips and techniques to correctly estimate the RAP via echocardiography:
- We estimate the RAP to help determine if a patient has pulmonary hypertension.
- The IVC helps to determine central venous pressure and central venous pressure is synonymous with RAP.
- The Collapsibility Index is the relationship between the diameter of the IVC and the percent collapse of the IVC during inspiration.
- Measure the diameter of the IVC 1-2 cm away from the right atrium.
- To accurately assess IVC collapsibility use M-Mode as it allows for better interrogation of the IVC over time and displays: pre sniff, sniff and post sniff views in the same image
- The sniff is preferred instead of a normal inspiration. Normal inspiration will not cause sufficient collapse of the IVC.
- The easiest way to remember the specific RAP values is to understand the opposite ends of the RAP spectrum – the normal versus high pressure. Everything else will just fall into the middle category.
- The RAP reference range is: Low = 3mmHg, Intermediate = 8mmHg, High = 15mmHg
CardioServ is an accreditation consulting firm specializing in full service accreditation as well as clinical development and education in diagnostic imaging. Sign up for our newsletter and follow us on Facebook to get the most up to date news on cardiovascular imaging!