 This week we are continuing the discussion of the movement in nuclear cardiology towards patient centered imaging and the emphasis on reduction of radiation exposure. Many organizations are changing guidelines and standards to align with these principles, one of them being the Intersocietal Accreditation Commission (IAC). Patient centered imaging is the focus of many changes in nuclear accreditation guidelines. In our last blog, we discussed 5 ways to reduce radiation exposure. IAC implemented all of these in their guidelines. Here is a quick review:
This week we are continuing the discussion of the movement in nuclear cardiology towards patient centered imaging and the emphasis on reduction of radiation exposure. Many organizations are changing guidelines and standards to align with these principles, one of them being the Intersocietal Accreditation Commission (IAC). Patient centered imaging is the focus of many changes in nuclear accreditation guidelines. In our last blog, we discussed 5 ways to reduce radiation exposure. IAC implemented all of these in their guidelines. Here is a quick review:
The main goal of this blog is to remind our readers: There is no protocol that is optimal for every patient. As medical providers, we should all strive to implement patient-centered imaging. If your facility is performing the same SPECT protocol for all patients there is room for improvement of patient care.
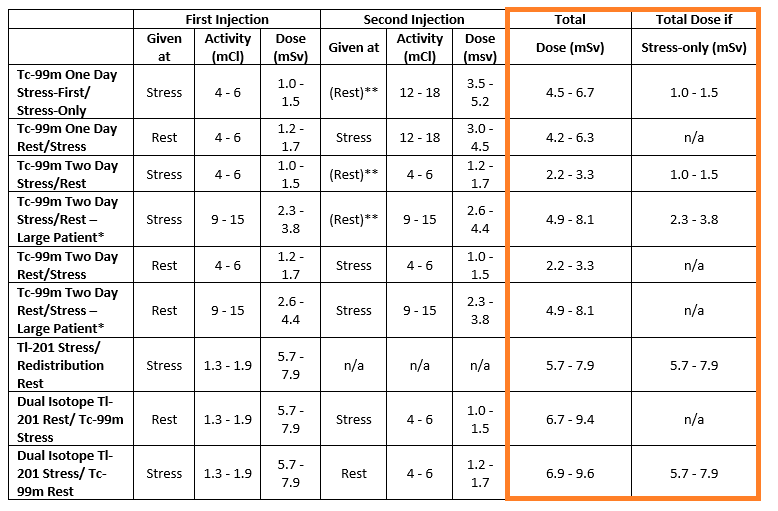
In February 2016, the American Society of Nuclear Cardiology (ASNC) released an updated Imaging Guidelines for Nuclear Cardiology Procedures. These guidelines included SPECT MPI imaging protocols with recommended effective doses. The table is broken down into the following sections:
When reviewing the effective dose reference table the following applies:
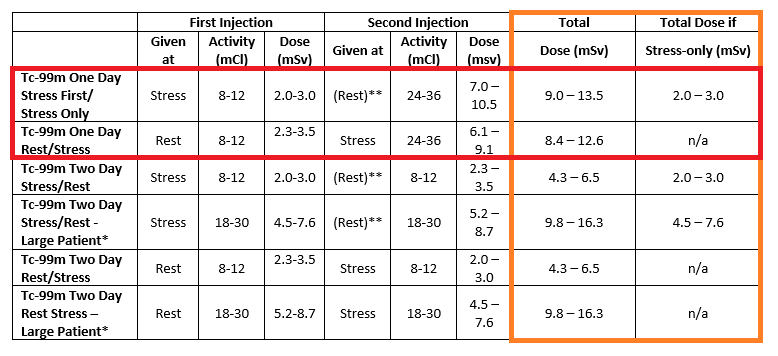
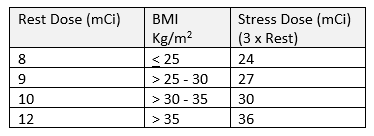
Tc-99m protocols are preferred as they have a shorter half-life while producing better quality images. The protocol and dosing amount should be tailored to the patient and the specific clinical situation. Using the example of a one day Stress/Rest protocol the table provides a Stress range of 8-12 and a Rest (if needed) range of 24-36. How do you determine the dose that’s best for your patient? Some labs use the following criteria for the resting dose with a stress dose of three times the rest:
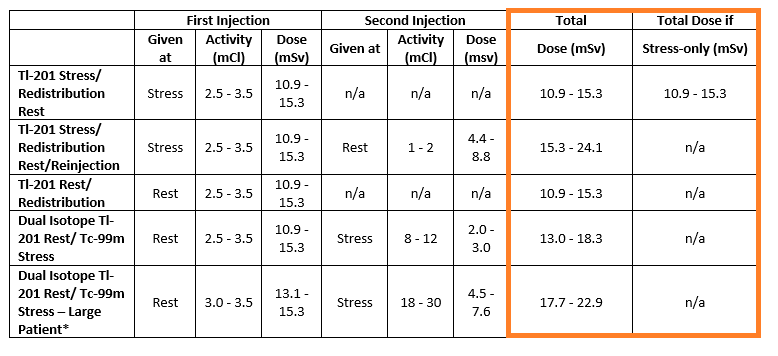
ASNC recommends against performing dual isotope myocardial perfusion imaging (MPI). There is significantly higher radiation dose to the patient and using different isotopes increases the false positive rate for ischemia
Newer iterative reconstruction software can optimize nuclear imaging reducing the time and/or dose administered. The software can be fitted on most existing systems if the gamma cameras are DICOM-compliant. Most major vendors offer technology with the systems. If your facility has not implemented this software, talk to your vendor about acquiring it.
If your facility is considering buying a new machine, there is newer hardware that can reduce radiation dose significantly. These include:
IAC updated their nuclear standards in September of 2016 that were in alignment with ASNC’s updates. The changes related to radiation safety include a focus on patient centered imaging and include:
Our goal is to ensure our patients receive radiation exposure As Low As Reasonably Possible (ALARA). ASNC states that a radiation effective dose of < 9 mSv in at least 50% of our studies is an extremely important goal for each laboratory to attain. What does that mean in everyday practice? If we look back at the table(s) above the total effective doses are highlighted in the orange boxes. If you pay attention to the one-day protocols often used in facilities (highlighted in the red box) you will notice the total effective dose for patients that receive both the stress and rest portion of their test is in the range of 8.4 – 13.5. Whereas patients that receive only the stress portion of their test receive a much lower dose of 2.0 – 3.0. In order for our labs to meet this extremely important ALARA goal we need to review our MPI protocols and ensure as many patients as possible only receive stress-only protocols.
Next week as we close out Radiation Safety Month at CardioServ we will review the new IAC Quality Improvement Guidelines and discuss how to incorporate Dose Verification assessment to meet your Technical Measure requirements.



